A FAMILY campaigning for an inquest into their father’s death claim an investigation that highlighted concerns about his medication plan was kept from them for months.
Alfie Hannaway from West Belfast had been on the blood thinning drug warfarin after undergoing major heart surgery at the Royal Victoria Hospital last year but died of a brain haemorrhage after being re-admitted a number of weeks later.
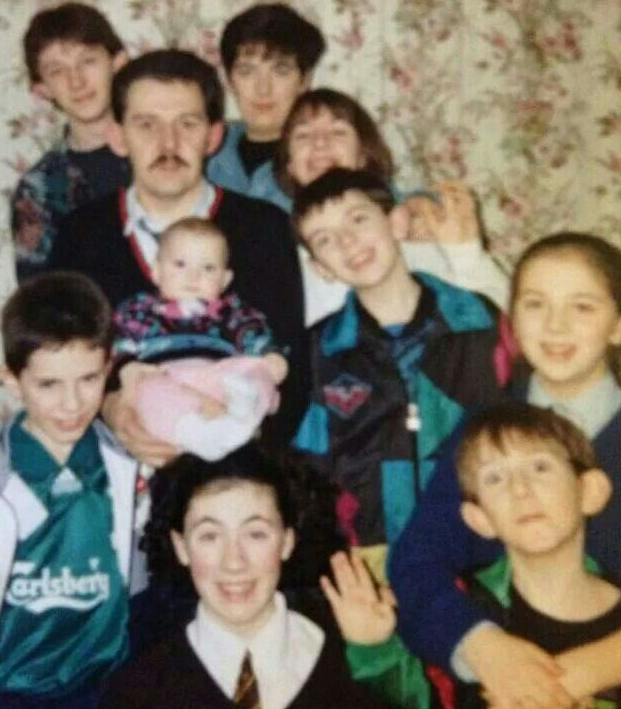
The father of eight and grandfather of 19 was 61 when he died.
In a letter to the family last month the Belfast Trust apologised and said: “There were serious deficiencies in the communication regarding your father’s surgery and discharge, and therefore his warfarin management following discharge.”
The case has emerged as The Detail can reveal that there has been a sharp increase in the number of Serious Adverse Incidents (SAI) taking place in in Northern Ireland’s health and social care settings.
This can include serious injury and controversial deaths.
An SAI investigation is a process designed to assess what has happened and decide what level of review is required.
A report from the Health and Social Care Board (HSCB) from June this year shows that from the beginning of October 2013 to the end of March 2014, there were 300 Serious Adverse Incidents reported. This represents a significant increase on the previous six months when 183 SAIs were reported.
A spokesperson for the HSCB said the increase can be explained by a number of factors including a change in reporting procedures. In a statement the board said the figures were “evidence of a more open learning culture, and increases the opportunity for improving patient and client care.”
Mr Hannaway’s death on 21 September 2013 was among the first group of hospital deaths investigated as part of new SAI procedures which were introduced in Northern Ireland at the end of last year.
The revised procedures emphasise the need for family involvement in investigations, but the Hannaway family say their experience has been one of “confusion and uncertainty”.
In November last year, as part of the SAI review into Mr Hannaway’s death, the Belfast Trust completed a report that highlighted concerns and made recommendations for learning regarding the management of his medication.
However the Hannaway family say they were not made aware of the report’s existence or its findings until March 2014.
Following reports of a number of high profile hospital deaths, the Health Minister, Edwin Poots, outlined to Stormont’s health committee in June 2014 that it was “not acceptable” when families are not kept fully informed about the progress of investigations into the standard of care of their loved ones.
Mr Hannaway’s death was not initially earmarked for further investigation by the Coroners’ Service for Northern Ireland.
However following the findings of the SAI investigation and a lengthy campaign by the family, their father’s case has since been re-opened by the coroner.
An investigation by the coroner is currently underway to determine whether or not an inquest should take place.
Coroners are independent judicial officers who deal with matters relating to deaths which may require further investigation to establish the cause of death. If there is evidence that a death was not from natural causes, then a coroner may decide to hold an inquest.
However Mr Hannaway’s son Alfie said the system has already failed his family.
He said: “We can clearly see that if it wasn’t for us pushing the issue, the coroner wouldn’t now be involved.
“There has to be something wrong with that system and that process has to be improved.
“Why should we, a bereaved family, have to try and chase these issues up?”
A spokesperson for the Health and Social Care Board (HSCB) said that the Hannaway’s description of their experience would “not be as expected” and that dealing with bereaved family members is a challenging area that requires “continuous improvement, feedback and support to staff”.
“WHATWENTWRONG?”Mr Hannaway had been on the drug warfarin to prepare for major heart surgery.
His dosage was written down in what is known as the patient’s “yellow book” which is used to record the monitoring of medication.
After surgery in September last year, Mr Hannaway was stabilised on a lower dosage of warfarin and was meant to be continued on this lower dosage after discharge.
Before leaving hospital he was given a new yellow book to reflect the updated lower dosage he required after surgery.
However his old yellow medication book with the higher dosage also remained in his possession when he was discharged. This was used as the current record by medical staff tasked to visit Mr Hannaway at home and take a blood sample following his surgery.
As Mr Hannaway could not attend the warfarin clinic in person for a prescription because of his recent surgery, the sample and the outdated yellow medication book were sent to the warfarin clinic and were used to calculate Mr Hannaway’s warfarin dosage.
The warfarin clinic continued on with this outdated regime unaware Mr Hannaway had undergone surgery.
Mr Hannaway therefore unknowingly continued to take the wrong pre-operation dosage of warfarin for a number of weeks until his final re-admission to the Royal on 21 September 2013 when he died.
A blood test used to monitor warfarin taken on the day of Mr Hannaways death, gave an abnormally high reading of 8.93, compared to a reading of 2.56 a number of weeks earlier.
In correspondence with the Hannaway family from July this year the Belfast Trust acknowledged that it was “the responsibility of the discharging ward to ensure adequate and timely communication to the warfarin clinic around monitoring and dosing post discharge.”
The trust said that in Mr Hannaway’s case the warfarin clinic did not receive the information which would have alerted them to the fact that he recently had surgery and would therefore not have been aware of any changes which might affect his warfarin dosage.
In the letter the trust acknowledged that for patients based in the community, it is generally not the practice of the warfarin clinic to seek further patient information when the medication dosage is being based on blood results alone.
The trust outlined that this practice has now been changed and that all warfarin clinic staff will now have access to an Electronic Care Record (ECR) system that was piloted last year, in order to enhance the availability of patient information.
“WE WERE SHOCKED”Mr Hannaway’s son Alfie said his family had no way of knowing at the time about the overdose which his father was taking.
He said: "When he was in hospital the lower dosage was obviously monitored very well. But when he was at home recovering, he had a visit from the medical staff and his warfarin dosage was increased when it shouldn’t have been.
“We had no reason to question the dosage because he had 100 percent faith in the doctors and nurses and wouldn’t question them. We assumed everything was OK.”
However just weeks after surgery, in the early hours of 21 September Mr Hannaway had to be re-admitted to the Royal Victoria Hospital with a brain bleed.
He passed away in hospital six hours later.
His family says they were initially led to believe that their father’s body would be the subject of a postmortem examination and his death may be investigated by the coroner.
However after considering the trust’s clinical summary and formulation of cause of death the coroner was content for the body to be released and a death certificate was issued.
A doctor for the trust wrote a medical death certificate which outlined that Mr Hannaway had been on warfarin, recently had surgery and that there had been a bleed into his brain associated with high blood pressure and an abnormal bleeding state.
Alfie says that in the immediate aftermath of his father’s death his family tried to understand what had happened.
He said: “Afterwards there was a lot of confusion and there was some talk by staff that the coroner would have to be spoken to and about a possible postmortem. But when we were making arrangements for daddy’s wake the undertaker told us that daddy’s body had already been released and that really shocked us.
“At this point we had no idea there were any issues with daddy’s warfarin, we didn’t know what signs to look for.”
Shortly after Mr Hannaway’s death, a family friend with experience of the same medication raised concerns about the fact that that he had two yellow warfarin books in use in the lead up to his death.
The family sought answers from the trust.
In a meeting with health officials three weeks after their father’s death, the Hannaway family raised concerns about the content of their father’s death certificate and why there had not been further investigations into what had caused his death.
They also asked questions about the association between the life-threatening bleed in their father’s brain and whether it could have been caused by too much warfarin.
The family say they were told by the trust that it would carry out an “informal fact finding exercise”.
However their persistence had in fact prompted a Serious Adverse Incident (SAI) investigation, but the family said they were only informed about the report and its findings months after the investigation had been completed.
In a statement to The Detail the Belfast Trust said: “We offer our sincere sympathy to the Hannaway family on the death of their father. While we are not in a position to discuss any individual’s treatment or care, we are in communication with the Hannaway family, and will continue to be so through to the outcome of any ongoing investigations.”
On 12 November 2013, Mr Hannaway’s death was reported to HSCB as a Serious Adverse Incident. A month earlier, in October 2013, there had been a complete overhaul of the SAI reporting system across Northern Ireland’s health and social care sector.
A single investigation process for all SAIs was replaced with three levels of SAI investigation:
- Level 1 is known as a Serious Event Audit (SEA). Its purpose is to establish quickly what has happened so that there can be early learning of lessons.
- Level 2 is a Root Cause Analysis (RCA) and is carried out by a team not directly involved in the incident. It Involves a more detailed investigation and final report must be submitted to the HSCB within 12 weeks of the incident.
- Level 3 investigations will be considered for SAIs that are particularly complex, have a degree of technical complexity that requires independent expert advice or are very high profile and attracting a high level of both public and media attention.
Mr Hannaway’s case was not pursued as a Level 2 or Level 3 investigation but a Serious Event Audit (SEA) report was carried out. The report was completed on 20 November 2013 and was sent to the HSCB on 11 December 2013.
However the Hannaway family say they were not made aware of the SEA report’s existence or findings until 3 March 2014.
“STRICT VIGILANCE”The report identified a number of failures in Mr Hannaway’s discharge and follow up arrangements at home in relation to the management of his warfarin.
It said that in the light of Mr Hannaway’s “unexpected death” the trust had concluded that “having more than one booklet for daily warfarin monitoring may lead to the wrong information being used by the district nurse and the warfarin clinic”.
The report stated there was no record in the outdated yellow book given to the warfarin clinic stating the fact that Mr Hannaway had just had surgery.
It states: “There was an assumption that the patient’s condition was unchanged as can happen when a result is based on a sample and not the patient. There may be reasons other than surgery such as an illness or change in other medications, which should be considered when prescribing warfarin and therefore it is inherently unsafe for the warfarin clinic to be expected to prescribe a dose of warfarin if a patient is not physically present at the clinic.”
The report concluded by stressing the importance of “strict vigilance” which is required when a patient is on warfarin and stated that the findings would be shared with the medical director, other wards, local and regional pharmacy groups as well as doctors in primary care.
A number of days after receiving the SEA report the Hannaway family met with the trust once again.
Mr Hannaway’s son Alfie recalls that the family still had a number of outstanding questions.
He said: "It became clear at the meeting that the trust hadn’t sent a copy or contacted the coroner about daddy’s SEA report at that stage, but we stressed that this was something we felt very strongly about.
“Also It wasn’t made clear to us during the meeting that the SEA report was actually part of a Serious Adverse Incident investigation. The first time we heard the term used was when the trust referred to ‘ongoing SAI investigations’ in a statement to The Detail in June this year.”
On 27 March 2014 the coroners’ service was sent a copy of the SEA report by the trust.
In correspondence with the family from May this year, the coroners’ service confirmed that the report highlighted a number of concerns regarding the management of their father’s warfarin and stated that as a result that it was reopening his case.
A decision is now pending on whether or not an inquest should be held into Mr Hannaway’s death.
“A SERIOUSERRORINVOLVINGYOUR FATHER”In a letter written to the family in July this year, the Belfast Trust apologised for the time taken to respond and said that in reviewing their father’s case it was clear there were “serious deficiencies” in the communication regarding his “surgery, discharge and therefore warfarin management”.
The trust said it hoped it had demonstrated how seriously it took the “serious error” involving Mr Hannaway.
However Mr Hannaway’s son, Alfie, says many questions remain unanswered.
He said: “We obviously feel that daddy’s death should have been investigated by the coroners’ service from the beginning and instead here we are almost a year later and that decision is still pending. We’re still not clear about why it has taken this long.
“There’s been so much confusion that we feel the only way that lessons can be learned in a public way is through an inquest.
“We’re lucky as a family that we are a strong unit and we can support each to push on, but other families may not be so lucky to have that support to get the answers that they as families deserve.”
INVESTIGATINGHOSPITALDEATHSA previous investigation by The Detail highlighted a number of cases where there had been delays in controversial hospital deaths being reported as SAIs and being reported late to the coroner.
In response to a number of Northern Ireland Assembly written questions on SAIs in May this year the Health Minister stated: “There are very limited circumstances when it may not be appropriate or responsible to advise a patient/family that a Serious Adverse Incident has occurred or where it would be appropriate to delay telling them and this is the position with some of these cases. The main reason is likely to relate to concerns with regard to the vulnerability or mental health and well-being either of patients or next of kin.
“I am determined to ensure that cases where patients or families are not told that a Serious Adverse Incident investigation is underway should be exceptional. I have instructed the HSCB to introduce new monitoring arrangements around the involvement of patients and families with Serious Adverse Incident investigations.”
Responsibility for SAI procedures lies with the Health and Social Care Board.
A HSCB Learning Report from June this year obtained by The Detail outlines that during the period 1 October 2013 to 31 March 2014, the HSCB received 300 SAI notifications.
This represents an increase on the previous six months (April 2013 – September 2013) when 183 SAIs notifications were reported to HSCB.
October 2013 to March 2014 was the first reporting period since the new SAI procedures were introduced. The board says this will have led to a “heightened awareness” from staff that will account for some of the increase in reporting.
The revised SAI procedure also includes a new policy that any death of a child up to age 18 in a hospital setting must be reported as an SAI. The board says this will also have had an impact on the number of SAIs reported during this period.
Since Mr Hannaway’s death the board says it has produced revised SAI documentation to include a checklist to identify family members as well reminding doctors of the statutory reporting to the coroner where there is a requirement to do so.
A spokesperson for the board said that Mr Hannaway’s SEA report would only be closed when health officials were “satisfied that all recommendations are being addressed”.
In a previous story we revealed that Northern Ireland’s Attorney General, John Larkin, had written to the Justice Committee seeking new investigative powers to force the release to his office of records linked to hospital tragedies, such as SAIs.
The power is to be considered as a possible amendment to the Legal Aid and Coroners’ Courts Bill. If granted it could see the Attorney General’s office scrutinising the paper work relating to all SAI deaths and on that basis directing an inquest where it is deemed further investigation is needed.
Alfie Hannaway believes that something needs to be done to prevent bereaved families going through a similar ordeal.
He said: “If it wasn’t for us pushing the trust on our father’s case we firmly believe the coroner wouldn’t be involved. There has to be something wrong with that system, the process has to be improved.
“If there is someone or else an organisation with independence who can come in with the investigatory powers to get this information, instead of us as a family trying to chase it, then that can only improve transparency.”
 By
By