By Niall McCracken
IMPORTANT measures to improve the care of newborn babies in Northern Ireland have not yet been put in place, despite deadlines set by the review team investigating the Pseudomonas outbreak.
Documents obtained in a Freedom of Information request show that a regional neonatal network in Northern Ireland which was due to be established by September this year is not yet in place.
Earlier this year the review team concluded that the current neonatal network operates on an “informal basis”. They recommended that a formal network should be established with agreements put in place to ensure resources across the region are “utilised to best effect, working to common policies and procedures.”
Furthermore, plans to put in place a 24 hour service for regional transfer facilities for new born babies failed to meet a July 2012 deadline. It currently operates at a 12-hour capacity.
The interim and final report of the “Independent Review of the Incidents of Pseudomonas Aeruginosa Infection in Neonatal Units in Northern Ireland” made a total of 32 recommendations. While most have been completed, The Detail has identified a number of significant outstanding issues.
To see a full copy of all the recommendations and the information obtained under FOI please click here. The information outlined is a summary of progress as of October 11 2012.
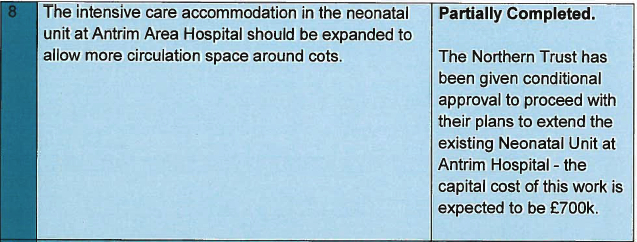
INTERIM REPORTRecommendation eight of the interim report outlined that the intensive care accommodation in the neonatal unit at Antrim Area Hospital should be expanded to allow more circulation space around cots:
However, in an updated statement regarding the neonatal unit at Antrim Area Hospital a spokesperson for the Department of Health Social Service and Public Safety (DHSSPS) said: “The response provided earlier erroneously indicated that the business case had been approved. This is not yet the case but work is on-going to secure early approval with a view to work commencing on site as soon as possible thereafter.”
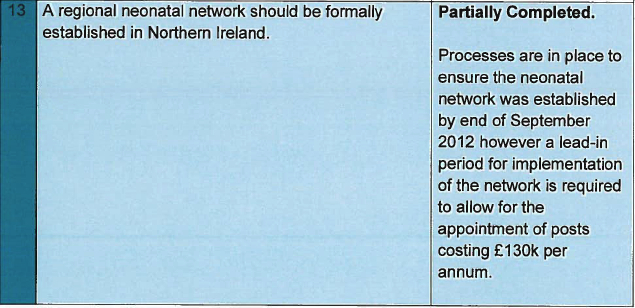
Recommendation 13 laid out plans to set up a regional neonatal network in Northern Ireland. This was originally to be completed by September 30 2012:
The department said that an informal neonatal network has been in operation for a number of years, but that “work continues to progress this to a formal network.”
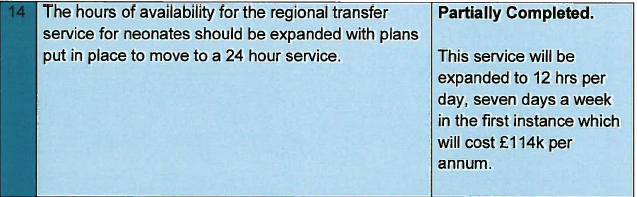
Recommendation 14 stated that the hours of availability for the regional transfer service for neonates should be expanded with plans put in place to move to a 24 hour service. It was recommended that this should be completed by July 31 2012:
A spokesperson for the department said that figures for 2011 indicate there were 15 transfers out of a total of around 500 outside the hours proposed but that “progress continues on expanding the hours of availability for the regional transfer service.”
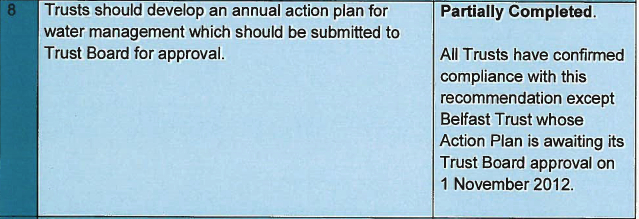
THE FINAL REPORTRecommendation eight of the final report outlined that trusts should develop an annual action plan for water management which should be submitted to the trust board for approval. Each trust was to provide approval by September 28 2012:
In a statement to The Detail the department said that the timing of the Trust Board’s formal approval has not “impeded the Trust’s implementation of the key actions that need to be put in place.”
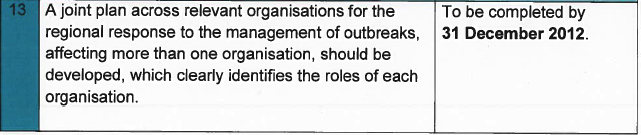
Recommendation 13 outlined the implementation of a plan across the relevant organisations for the regional response to the management of outbreaks, affecting more than one organisation:
Other recommendations that are due to be completed by December 31 2012 are guidelines for the organisation of regional teleconferences for future incidents.
HEALTH PROTECTION AGENCY FINDINGSTHE findings of a Health Protection Agency (HPA) report which was published just days before the publication of the RQIA led review into the Pseudomonas outbreak, sheds new light on some of the information that circulated in the aftermath of the baby deaths earlier this year.
The in-depth document was overshadowed by the Troop Review’s findings which would come in for criticism from some of the families for not addressing their key concerns.
The HPA report from May 2012 questions whether or not the taps were the source of patient contamination, or if an external factor resulted in the contamination of both patients and taps.
It also queries the effectiveness of the “deep cleaning processes” that took place within neonatal wards following confirmation of the outbreak.
And it provides further analysis on the use of sensor taps and reports that almost 80% of the taps that were received for analysis following the outbreak were of a design that had a greater probability for being colonised with pseudomonas.
THE SOURCEThe Regulation and Quality Improvement Authority (RQIA) published its final report on May 31 2012 and concluded that the outbreaks were linked to contaminated tap water in the intensive care rooms of the affected neonatal units and that the most likely method spread of the infection to the babies was the use of tap water in washing during nappy changes.
The HPA’s “Investigation of Pseudomonas aeruginosa on biofilms in water tap assemblies from Neonatal Units in Northern Ireland” from May 29, provides a more detailed analysis of the design of the taps and points to the “Rosette” or “flow straightener” – a single component which sits at the end of the tap outlet.
It highlights further questions that remain unanswered about where the contamination originated from. It states:
“Whilst the rosette components were contaminated with the same P. aeruginosa (Pseudomonas) isolates that were also recovered from patients, it is not possible to determine from these data whether the taps were the source of patient contamination, or whether an external factor resulted in the contamination of both patients and taps.”
In a statement to The Detail, the Department said: “Psuedomonas aeruginosa is present in the general environment and can be carried on the skin and clothing. Being an opportunistic pathogen, it can colonise and form biofilms in areas that are provide warmth and oxygen. If this occurs, as HPA have stated, water may have been the vehicle of transmission of the pathogen.”
THE DEEP CLEANThe HPA report also summarises how in an attempt to reduce potential colonisation, the single component which sits at the end of sensor was removed from some taps in the neonatal units, but that this led to splashing in the sink area resulting in health and safety issues and increased the risk of contamination.
Following confirmation of the Pseudomonas outbreak at the Royal Jubilee Maternity ward, staff carried out a “deep clean” at the hospital’s neonatal rooms on January 21 2012.
The HPA’s investigation however, casts doubt over the effectiveness of this method: “Taps from the neonatal unit in Belfast had been exposed to a deep clean using vaporised hydrogen peroxide prior to removal and replacement.
“Whilst this may have reduced counts on the outside collar of the rosette, the recovery of P. aeruginosa demonstrates that biofilms are not only persistent but also resistant to such deep cleaning processes and raises issues about the efficacy of such processes.”
SENSOR TAPSThe RQIA report highlighted concerns about links between sensor taps and Pseudomonas infection and point out that there has been considerable debate regarding which design of tap is most likely to protect the water system from bacterial contamination.
The HPA’s report goes further. To assess the presence of Pseudomonas, they examined the various tap assembly components from neonatal wards across Northern Ireland following the four fatal cases. Its study highlights that the sensor taps (all of a single brand) accounted for 79% of the tap assemblies that were received for analysis and the results indicated that these sensor taps had a greater probability for being “colonised” with Pseudomonas and had a higher Pseudomonas count than the non-sensor taps analysed
The study also shows that even when the tap body has been replace there is still a risk of further contamination:
“The removal and replacement of the rosette and metal collar will still leave behind a P.aeruginosa (Pseudomonas) biofilm on the tap body. Therefore, this may explain why replacing the tap body is one of the ways of controlling the presence of P. aeruginosa in water samples from such outlets.
“However, as the results have shown, even where the tap body has been replaced there may still be contamination of other components such as the flexible tubes and thermostatic mixer valve. These contaminated components would also lead to biofilm being sloughed off that would result in sporadic P. aeruginosa counts in water samples and would, within a few weeks, also result in the contamination of the new tap body and rosette.”
The department say it is because of this position that guidance issued by DHSSPS during the outbreak outlined that all taps in neonatal units should be replaced with manually operated lever taps and that all flexible hoses, plastic components, thermostatic mixing valves and isolating valves be removed.
At the end of January, Health Minister Edwin Poots announced that taps in all neonatal units in the region would be replaced. The department have confirmed to The Detail that the “majority of the taps” in Northern Ireland’s neonatal units are now manually operated twin lever mixer taps from various manufacturers. While the Royal Group of Hospitals have installed a “number of taps” incorporating UV technology.
These responses do not make it clear what outstanding work still needs to be carried out in Northern Ireland’s hospitals.
The RQIA has confirmed that they have developed a new draft neonatal infection prevention and control audit tool and are in the process of conducting a series of evaluation visits to neonatal units across Northern Ireland.
At the same time The Department of Health, Social Services and Public Safety has launched a consultation on a draft policy for cleanliness in the Health & Social Care (HSC) sector in Northern Ireland. The draft policy is out for 13 week consultation which will close on November 2 2012.
 By
By